The Human Heart Parts and Structure - Biological Anatomy
The heart structure consists of connective tissue and cardiac muscles. The latter is a type of involuntary muscle. Here are some interesting facts about the heart's parts and functions. The cardiac muscle contracts and relaxes independently without requiring you to apply force deliberately.
Your heart is a delicate organ. Any damage to it will cause an interruption in the heart's functions. So, it gets protection from the rib cage. Concerning shape, it looks like a cone. The base of this cone is positioned upward and gradually tapers down to the apex.
The pumping organ is roughly the size of a wrist. It measures 12 cm, 8 cm, and 6 cm along the length, width, and thickness, respectively. The effect of the exercise on the muscles of the heart organ is the same as shown by the skeletal muscles.
That is, as an outcome of exercise, they grow both in size and strength. That is why well-trained athletes usually have much larger hearts. Such a thing also enhances heart function.
1. Cardiac Chambers
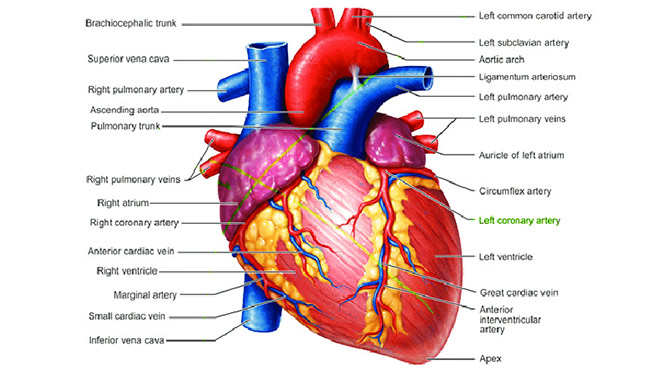
While a frog’s heart is 3-chambered, a human heart has 4 chambers. The upper 2 chambers are called the left and right atria. The lower 2 chambers are called the left and right ventricles. The right atrium and ventricle contain oxygen-depleted blood collected from the upper and lower parts of the body through the superior and inferior vena cavae.
On the other hand, the left atrium and ventricle contain oxygen-rich blood, which is pumped through the whole body through the aorta.
2. Heart Layers
The inner lining, the heart muscle, and the outer covering are the 3 major layers of the heart. These layers are called endocardium (inner), myocardium (middle), and pericardium (outer). The outer layer or pericardium can be distinguished into an outer lining or epicardium and a loose sac.
Pacemakers
You might know all cells within your heart’s conducting system can activate electrical impulses. While some are actively involved in the rhythmic contractions, others usually serve as standby pacemakers. In other words, different accumulations of cells or pacemakers are activated at different times in priority order. Researchers have identified three types of pacemakers in your heart, i.e., primary, secondary, and tertiary.
1. Primary Pacemaker:
The SA node has been designated as the leading primary pacemaker due to the highest discharge rate. The SA or sinoatrial node is found at the junction of the right atrium and the superior vena cava. Discharging the electrical potential from the SA node or the primary pacemaker activates the conduction system.
An electrical impulse traveling through the conducting system induces contraction of the cardiac muscle. The discharge of electrical potential is termed as depolarization. After depolarization, the specialized cells in the SA node start rebuilding electrical potential for the next impulse.
The regeneration of electrical potential is called repolarization. You can note that the depolarization and repolarization in the heart are analogous to the discharge and recharge of a battery!
2. Secondary Pacemaker:
The secondary pacemaker consists of the lower part of the AV node at its junction with the bundle of His. You can locate the AV node in the lower septal wall of the atrium. The bundle of His emerges from the lower part of the AV node and enters the junction between the ventricles and the atria. Compared with the primary one, its discharge rate is considerably low – just around 50 times/min. It is activated only when its primary counterpart stops to discharge.
3. Tertiary Pacemaker:
When the primary and secondary impulse formation systems stop working, the tertiary pacemaker assumes its role. It is the tertiary center in the ventricular conducting system. The tertiary pacemaker acts as the 3rd line of defense against the impulse's failure to reach the heart's lower chambers.
The tertiary pacemaker consists of the lower divisions of the conducting system, including the Purkinje network. The Purkinje network is formed from the division and subdivision of the principal branches (left and right bundle branches) of the bundle of His.
Being slower than that of both the primary and secondary pacemakers, its discharge rate is just about 30 to 40 times per minute. An interruption in the connection between the Purkinje system and the AV node triggers the activation of the tertiary impulse formation unit.
In this case, the atria and the ventricles contract at different rates. It is because, obeying the primary pacemaker, the atria contract faster. And, under the influence of the tertiary pacemaker, the ventricles contract at a slower pace.
Heart Valves:
To separately manage systemic and pulmonary circulations, your heart needs to maintain the unidirectional flow of the blood. A few-word answer to “What is the function of the heart valves?” is they maintain a one-way blood flow. So, they act like check valves, similar to those installed in the water supply system in your home.
The 4 heart valves are bicuspid, tricuspid, pulmonary, and aortic. Two of them are located between the heart chambers to control blood flow from the atria to the ventricles. The remaining two valves – pulmonary and aortic – control the blood flow out of the ventricles.
1. The Mitral Valve:
Consisting of two leaflets, it is also called a bicuspid valve. It is located between the left atrium and the left ventricle. The mitral valve prevents the backflow of blood from the lower left chamber to the upper left chamber.
2. The Tricuspid Valve:
Having 3 leaflets, the tricuspid valve is located between the right atrium and the right ventricle. It stops the flow of deoxygenated blood back from the lower right chamber to the upper right chamber. The tricuspid valve regulates the pulmonary blood flow.
3. The Pulmonary Valve:
This check valve is at the junction between the pulmonary artery and the right ventricle. In the presence of this valve, the oxygen-depleted blood from the pulmonary artery does not leak into the heart's lower right chamber.
4. The Aortic Valve:
Located between the largest artery – the aorta – and the left ventricle, the aortic valve regulates the flow of oxygen-rich blood from the heart to the various tissues and organs of the body.
Coronary Arteries and Veins
The coronary arteries and veins collectively comprise the blood circulatory network dedicated to the heart muscle. Like other arteries, the coronary arteries too contain oxygenated blood. Similarly, the coronary veins collect deoxygenated blood from the heart tissue and carry it to the right atrium for oxygenation.
Heart’s Functional Anatomy:
Sound knowledge of the heart’s functional anatomy would help you maintain and enjoy cardiac health. The heart functions involve the supply of oxygenated blood to all parts of the body. The circulatory system consists of three main types of blood vessels: arteries, veins, and capillaries. Arteries carry oxygenated blood and distribute it to different parts of the body.
On the other hand, the veins receive unclean blood, containing carbon dioxide and waste products, from the body parts and take it back to the heart. The heart contains both oxygenated and deoxygenated blood. It is its job to keep both separately in order to avoid contamination of the pureblood.
The heart's right chambers receive blood, devoid of oxygen, from the veins. This blood then goes to the lungs to receive oxygen and eliminate carbon dioxide. Afterward, this oxygen-rich blood returns to the heart, reaching all body parts through the arteries. In this way, every individual cell can get oxygen.
This oxygen will assist in the process of extracting energy from food. Read on for a detailed explanation of “How does the heart function?”
A double-walled membrane, the pericardium, separates the right and left chambers. That prevents oxygen-rich blood from mixing up with the one without oxygen. So, the heart functions go smoothly. Deoxygenated blood enters the right atrium. The valve present between the right atrium and the right ventricle is the tricuspid valve. It opens to let the blood flow into the right ventricle. The valve then closes to prevent the backward flow of the blood.
This deoxygenated blood enters the pulmonary artery and moves to the lungs to replenish its oxygen content. This oxygen-rich blood then comes back to the heart through the pulmonary vein. The left atrium welcomes this oxygenated blood into its cavity. The mitral valve between the left atrium and the left ventricle opens to let the blood flow into the left ventricle.
It then closes to prevent the backward flow of blood. Finally, the blood is pumped into the aorta, from where it is distributed to the rest of the body through the arteries. So, you can say that the heart's main function is to supply all the body cells with oxygen and nutrients through the circulatory network.